The goal of our research is to promote recovery of functional movement following spinal cord injury.
The spinal cord contains neuronal networks that have the capacity to generate many basic motor functions, including standing and walking. The focus of our lab is to understand how this intrinsic spinal cord capacity can be harnessed after spinal cord injury to promote recovery. With spinal cord injury descending control from the brain is lost, and so many neurons below the injury, including motoneurons, loose synaptic inputs that enable them the initiate and maintain activity. However, our recent work, in collaboration with the Fouad and Heckman labs, has shown that there are remarkable spontaneous adaptions of receptors (5-HT2C) and channels (calcium) in neurons below the injury, which enable these neurons to function autonomously, without control from the brain (Murray et al. 2010). These adaptations enable recovery of locomotion, but also lead to uncontrolled motoneuron firing and muscle spasms. Our ongoing work employs pharmacological and genetic approaches to guide these spontaneous adaptations to optimally promote locomotion and minimize spasticity, with the ultimate goal of designing new therapies for spinal cord injury.
Overall, we believe that understanding the naturally occurring repair mechanisms of the CNS provides an opportunity to develop future treatments for injuries and disorders of the entire nervous system. Our results demonstrate that functional benefits are not inevitably based on plasticity or regeneration of descending input from the brain, but can be caused by changing the activity of receptors and neurons below the level of the injury.
In our lab we explore methods to promote this spontaneous adaptation and recovery, to develop new therapeutic treatments for spinal cord injury, focusing on the following strategies:
1) Understanding the spontaneous changes in motor neurons below the injury, and attempting to promote this natural plasticity. For this, we are employing pharmacological methods to promote useful muscle contractions produced by these neurons, while minimizing unwanted muscle spasms. At the molecular level, we focus on understanding changes in channels and receptors on motor neurons after spinal cord injury.
4) Understanding how the peripheral nervous system compensates for spinal cord injury, including changes in the muscle properties. We have found that spasticity in muscles can help preserve muscle mass and function, even though it may at times impede movement.
Methodology
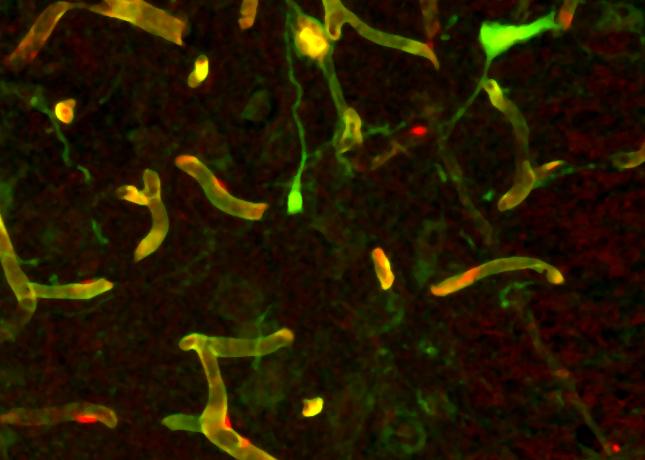
A major obstacle to understanding and treating spinal cord injury and spasticity in humans has been the lack of an adequate animal model of this condition. However, we have discovered that a sacral spinal cord transection (at S2) produces a pathology in the tail muscles of rats that includes many of the classical signs of the spasticity syndrome (hyper-reflexia, hypertonus, clonus, muscle spasms and delayed onset of about 1 month), with a remarkable resemblance to spasticity seen in the limbs of humans after injury (Bennett et al. 1999, 2004). This rat model is minimally invasive, only affecting tail muscles, and leaving normal hindlimb and bladder function fully functional, minimizing the need for extensive post-operative care. Importantly, we find that the entire affected spinal cord below the sacral injury site is small enough to survive whole (unsliced) when it is removed and maintained in vitro, regardless of the rat’s age after injury (Li et al. 2004b), allowing us to study spasticity in dish with detailed pharmacological methods. We have also found that this sacral cord can exhibit left-right rhythmic activity, allowing us to study rhythmic locomotor activity in adult rats in vitro. Other laboratories are only able to study chronic injury and spasticity in vivo, because in vitro methods have previously been limited to rats younger than 2 - 3 weeks, far too young to study spasticity, which takes months to develop. With these technical advances, my lab is rapidly unraveling the long-standing mystery of what causes spasticity and impairment of basic functions like walking. Our parallel studies in awake spastic rats and humans ultimately link changes in receptor and channel properties to motor function and treatment of spasticity in humans.
Facilities
Our facilities include a laboratory fully equipped for surgeries, physiological and pharmacological experiments, immunohistochemistry, molecular methods, and behavioural testing in rats.
Funding
We would like to acknowledge generous funding support over the years from the
- Canadian Institutes of Health Research (CIHR)
- Alberta Heritage Foundation for Medical Research (AHFMR)
- Natural Sciences and Engineering Research Council (NSERC)
- NIH
- Canadian Foundation for Innovation (CFI)
- Barbara Turnbull Foundation